The treatment of infantile colic – is it reflux, intolerance or GOR?
You have sailed through nine months of pregnancy amidst all the morning sickness, preparation, adjustments, worries and concerns that go with growing a human inside you. You have brought an amazing little human being into the world and as the books tell you, you should be in baby bliss right now, right?
BUT YOURE NOT!
Your baby is far from anything you have ever read about, imagined or dreamed of. You haven’t strung more than three hours of sleep together in the last month and your baby seems capable of screaming their little lungs out, absolutely inconsolable whilst you are treading a pathway of wear and tear through your carpet for it seems like 26 hours out of every day, scared to put him (or her) down in case they start yodelling again.
WAHT IS WRONG WITH MY BABY?
Its clear from your baby’s behaviour and their bowel habits that there is something wrong in their gut. They scream before a feed from hunger and after the feed from pain. Or they just sceam, drawing their legs up into their abdomen whilst passing or pooping smelly wind or faeces. Often this behaviour is characteristically in the afternoon between 4pm and 7pm, and after a period of time baby can spontaneously settle until this time tomorrow when it all happens again. Or else your baby screams after every feed and simply does not settle at all.
This article will seek to explain some of your baby’s behaviour why it happens & the actual physiology behind it, and what your doctor can do about it, form a biomedical viewpoint. Additionally, a naturopathic approach to this problem is also included along with some dietary advice and herbal remedies for both mum and baby to help settle that immature baby GIT.
What usually constitutes GIT disturbance?
The three most commonly accepted states to consider are: (a) Colic (b) Lactose Intolerance (c) Gastro Oesophageal Reflux (GOR)
Colic is the popular term used almost universally to describe unsettled behaviour in infants. This usually refers to bouts of seemingly inconsolable crying due to gastro-intestinal pain, which may be accompanied by abdominal distention (with flatus), vomiting, copious and loose stools and a tendency to draw up the legs. Severe cases also see other signs such as arching of the back and severe difficulty in settling. It usually resolves spontaneously at about 3 months of age. Parents need reassurance and practical suggestions on how to plan around the sessions of periodic crying which usually have a set time; the most characteristic being in the early evening.
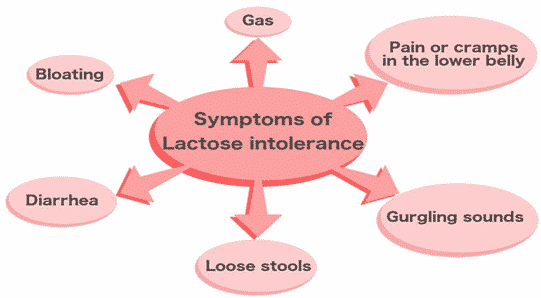
Lactose intolerance, (often diagnosed in the clinical setting by virtue of testing faecal pH and faecal reducing sugars or by the breath hydrogen test; but only truly diagnosed through a biopsy of the small intestine) manifests with chronic diarrhoea and a failure to thrive. In this situation the stool is characteristically frothy, watery and passed with much flatus. It is due to an inability to digest lactose, which is the primary carbohydrate in milk. The lactose levels in human milk are higher than in most other mammalian milks, the sugar being hydrolysed by lactase- phlorizin hydrolase, an enzyme in the small intestine. This enzyme develops in the neonatal gut mainly throughout the last trimester. By 34 weeks gestation, lactase activity is approximately one third that of the full-term infant reaching 70% of full-term level by 38 weeks’ gestation. Congenital lactase deficiency is extremely rare and is inherited as an autosomal recessive gene. Symptoms, therefore, are most likely to occur in premature infants or in those who have had undergone a bout of excessive peristaltic activity.
With either of these two conditions, the Lactation Consultant (LC) can offer assistance by suggesting feeding protocols such as timed and/or evenly spaced feeds designed to reduce excessive intake of milk and upright feeding positions. Encouraging the mother to allow the baby to ‘finish the first breast first’ increases the fat intake, which tends to reduce gut motility. This management technique is most effective when accompanied by dietary advice aimed at increasing the intake of mono and poly-unsaturated fats. Similarly increasing protein and complex carbohydrates at the expense of simple carbohydrates has been shown to decrease the lactose levels in human milk and, along with that, the common symptoms of lactose intolerance.
Parents appreciate also the practical advice and support offered by community groups such as NMAA (Nursing Mothers Association of Australia) and VISA (Vomiting Information and Support Association) who call upon a wealth of experience to share with parents thus assisting them to survive those early difficult weeks.
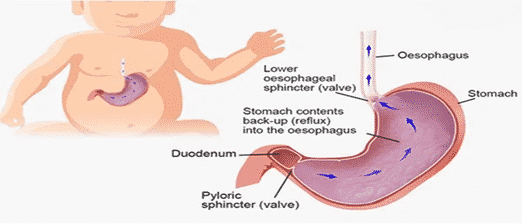
Gastro-oesophageal reflux is described as a pattern of consistent regurgitation leading to distress after feeds. In severe cases it may lead to apnoea, pneumonia, failure to thrive and anaemia. Oesophagitis (inflammation of the oesophagus) has been associated with candida and herpes. Mapping of a gene for severe paediatric gastro oesophageal reflux to chromosome 13q14 was published in the July 19, 2000 issue of The Journal of the American Medical Association where it was described as a common medical problem affecting one in 20 babies.
In the general population oesophageal reflux has been assessed as being prevalent in 4% of the population. Notionally it shouldn’t occur because of the presence of the lower oesophageal sphincter. Strictly speaking this is not so much a physiological entity as a zone of high pressure, which is maintained just above the gastro-intestinal junction. Normally this area has a high resting tension, which prevents or inhibits reflux. The sphincter usually relaxes once the peristaltic wave arrives. It is controlled by nervous and hormonal mechanisms. In adults this oesophageal pressure may be lowered due to cigarettes, alcohol, fat, caffeine and perhaps obesity.
However, it is acknowledged that a persistent pattern may occur in the first year of life due to a functional immaturity of the lower oesophageal sphincter leading to episodes of inappropriate relaxation.
A short intra-abdominal length of oesophagus as occurs in babies, probably also contributes to the problem. Also increased abdominal pressure resulting from fermentation in the small intestine due to problems coping with the daily lactose load in the still-maturing gut can be a significant factor. This tends to be exacerbated by the tendency for the baby to draw up the legs in response to pain. It is recognised that lying down also enhances intra-abdominal pressure. This becomes somewhat of an occupational hazard for pre-ambulatory infants. In those cases where the mother has a problem with copious supply and/or a vigorous letdown, the peristaltic wave tends to be enhanced giving little time for the sphincter to self-regulate appropriately.
Current paediatric protocols include:
- reassurance
- avoidance of over-feeding
- maintenance of a 30-degree head up prone position after feeds.
- Placing baby on the L side (in a sling) with the mattress raised for sleeping.
- antacids such as Gaviscon. Such alginate preparations form a gel on the surface of the gastric contents thus preventing reflux in the upright position.
- feed thickeners such as Carobel – not generally recommended unless severely distressed and unsettled, underweight and malnourished.
- early solids
- histamine receptor antagonists which lower production of acid and pepsin such as Cimetidine.
- Dopamine receptor antagonist drugs which increase the contraction of the lower oesophageal sphincter as well as promote gastric emptying, such as Metoclopramide. Metoclopramide does not promote gastric secretions.
- Cisapride stimulates acetylcholine release in the myenteric plexus in the upper GI tract. This raises oesophageal sphincter pressure and increases gut motility. Side effects may include diarrhoea, abdominal cramps and tachycardia.
It has been suggested that the successful use of Metoclopramide in alleviating the symptoms of oesophageal reflux can be considered as being equally confirmatory [as an endoscopy] for the condition. However, most paediatric texts advise 24 Hr ambulatory oesophageal pH monitoring, endoscopy and barium studies to rule out underlying anatomical abnormalities in the oesophagus, stomach and duodenum.
To minimise possible GIT disturbance in neonates, research, which offers possible screening assistance, is now beginning to appear in the lactation literature. Some of this revolves around the role that allergy plays in gastro-intestinal morbidity. Early studies have established that up to 50% of newborns presenting for paediatric assistance have a family history of allergy and have established the concept of a recessive mode of inheritance.
Other studies have determined elevated levels of IgE (Immunoglobulin E) in cord blood as early as 11 weeks gestation and cord serum total IgE levels of greater than 100U/ml are associated with 5 to 10 times greater risk for allergy than those of lower levels. In particular, cord serum levels of IgE above a level of 0.7 U/ml are significant predictors of subsequent allergy. Enhanced hemagglutinating antibody titres against lactalbumin and soybean have been detected in amniotic fluid. It has, therefore, been suggested that assessment of the amniotic fluid may also be a reliable predictor of possible allergy.
Human milk contains a plethora of immunologically and pharmacologically active components and hormones, which offer a significant level of protection to the developing neonate. The immunoglobulins, particularly sIgA, (Secretory immunoglobulin A) afford quite specific protection. At birth, when the neonate is most vulnerable to infection, the levels of sIgA in colostrum are three times higher than those found in mature milk. They persist, however, at significant levels throughout the lactation rising slightly (along with lactoferrin and lysozyme) during weaning. They provide protection against a range of bacterial and viral assaults. However their levels are influenced by maternal exposure to antigens and reflect the antigenic load in her gut. One study has been published correlating low levels of sIgA in colostrum with subsequent cow’s milk allergy.
Dietary antigens most associated with an allergic response evolve from cow’s milk, eggs, fish, beef and peanuts. Avoidance of these foods in pregnancy was once thought to infer protection for your baby, but most recent thinking is that there is no risk to baby if you eat these foods during pregnancy. Furthermore, introducing these foods into your baby’s diet early when solids are introduced, and exposing them allows the child to build a tolerance not an allergic response to these allergic foods. Having said that it must be mentioned here that if any immediate family member of yours has serious allergic responses or allergic episodes, then care should be taken accordingly in introducing your child to these allergic foods.
Clinicians who place value on this research tend to develop strategies to reduce allergenic load through environmental manipulation emphasising restrictive dietary protocols and promoting exclusive breastfeeding.
There are various hands-on modalities, which can offer another type of assistance to babies in distress. These include: Massage (perhaps with Aromatherapy oils); Bowen technique; Chiropractic or Osteopathy. If the birth has been, in any way, traumatic, any of these modalities are worthy of consideration.
NOW FROM A NATUROPATHIC VIEW…….
A naturopathic approach to GOR would be to concentrate on improving digestion. A grand elimination diet wouldn’t be suggested during lactation. However, removal of cow’s milk and/or soy proteins from the maternal diet does much to improve the clinical picture. Increasingly wheat is also seen to be problematical and a naturopathic approach would consider using a blood type diet. Without going into too much detail this dietary approach is based on the notion that blood types O and A are the earliest recorded blood types. Type O is referred to as the cave man blood type, while type A evolved during the period of settlement along the Tigrus and Euphrates rivers. Neither of these blood types tolerates dairy or wheat.
Treatment of colic also warrants the use of probiotic strains for the infant gut as well as using herbal carminatives and anti-spasmodics to relax smooth muscle spasm and assist in expelling excess wind from the gut.
The naturopathic approach to settling gut inflammation is with the use of Ulmus Rubra or Slippery Elm Bark, which may be administered quite safely to the baby. In King’s Medical Dispensary (the pharmacopoeia of the American Eclectic Physicians from the last century), Slippery Elm is described as “a nutritive, expectorant, diuretic, demulcent and emollient which is a very valuable remedial agent in mucous inflammations of the lungs, bowels, stomach, bladder or kidneys when used freely in the form of a mucilaginous drink”.
Its’ use today is relegated primarily to treating the gut because of its mucilaginous properties. It enjoys much success as a method of treatment for worms and dysentery when used aggressively as a gruel. However, for babies it can safely be given in the form of a thin paste mixed with EBM and administered by spoon from an eggcup. In those cases where familial eczema is a feature and salicylate sensitivity may be a problem, it is best to first mix a good pinch of the powder to a firm paste with boiling water and then add EBM when cooled. It tastes like dirt and tubercular babies tend to like it. It goes straight through the system and renders the characteristically watery stool of a baby with GIT disturbance, markedly thicker.
In those instances when early solids or feed thickeners are being considered, Slippery Elm Bark is a safe, effective alternative based on over 100 years of proven clinical experience. In those instances where gut problems arise after antibiotic use, a pinch of Slippery Elm Bark mixed with boiling water and then thinned out with EBM, three times a day for three days followed by a few doses to which a pinch of Bifidus powder (a probiotic) has been added can be most beneficial.
